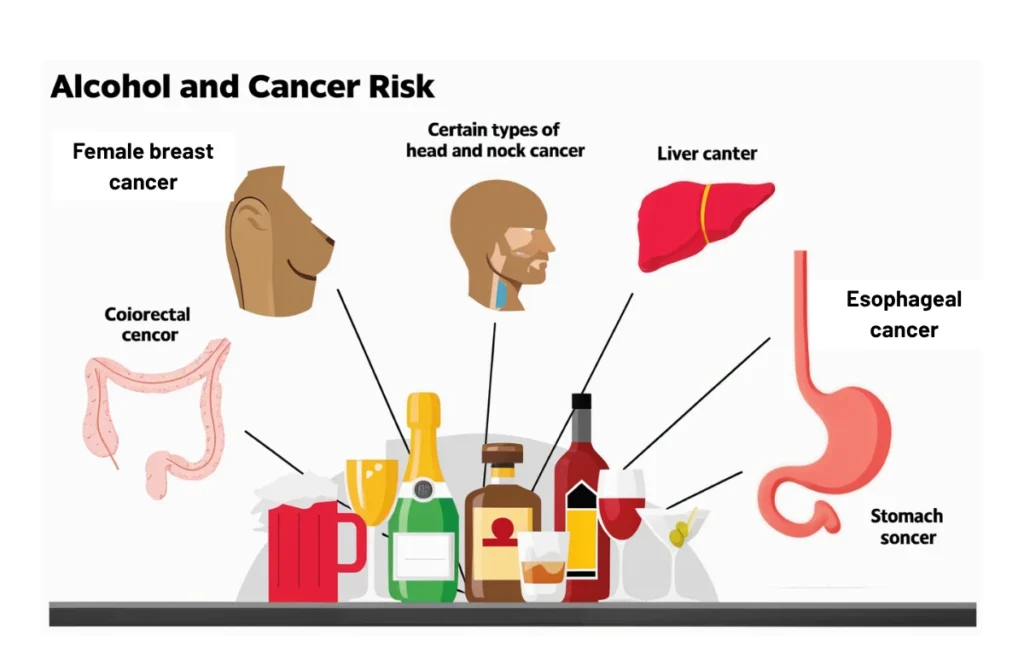
Colorectal cancer and alcohol use are crucial topics when discussing cancer prevention. The relationship between alcohol consumption and colorectal cancer has raised concerns among health experts and the general public alike. At The Arc Gut Clinic, we are dedicated to providing you with clear, evidence-based information on the risks and prevention strategies associated of alcohol and colorectal cancer
How Does Alcohol Affect Your Risk of Colorectal Cancer?
- Increased risk with alcohol consumption: Colorectal cancer and alcohol use have been shown to be linked. Drinking alcohol, especially in large quantities over an extended period, can significantly increase the risk of developing colorectal cancer. Alcohol has the potential to damage cells in the digestive tract, contributing to the formation of cancer cells.
- The role of acetaldehyde: When alcohol is metabolized in the body, it turns into acetaldehyde, a substance that is toxic and can damage the DNA within cells. This can lead to mutations that might result in colorectal cancer.
- Inflammation and cancer risk: Chronic alcohol consumption leads to inflammation in the gastrointestinal system. This inflammation can promote cancer development by altering the environment in the colon and rectum. The longer alcohol use continues, the higher the risk of colorectal cancer.
Alcohol Use Disorder and Colorectal Cancer
- What is alcohol use disorder? Alcohol use disorder (AUD) refers to a pattern of drinking that leads to significant distress or harm. Individuals with AUD are more likely to engage in heavy drinking, which is a known risk factor for colorectal cancer and alcohol use.
- Long-term effects of AUD on colorectal cancer risk: Those suffering from AUD typically drink large amounts over long periods, which increases their risk of colorectal cancer. The repeated damage caused by alcohol to the digestive system over time heightens the chance of developing cancer in the colon or rectum.
- Psychological and physical impacts: Alcohol use disorder not only harms the liver but also interferes with the digestive system’s ability to function optimally. This disruption may contribute to the development of colorectal cancer. Moreover, the risk is heightened due to the reduced ability of the body to repair the damage alcohol causes.
Explore our Lifestyle Counselling in Chennai to learn how personalized guidance can help reduce alcohol-related risks.
Heavy Drinking and Colorectal Cancer
- What is considered heavy drinking? Heavy drinking is defined as consuming more than three drinks per day, a behavior that has been linked to an increased risk of colorectal cancer and alcohol consumption populations to molecules
- How heavy drinking increases risk: Consistently heavy drinking can damage the digestive tract’s cells, causing inflammation and oxidative stress, which can lead to colon cancer and alcohol abuse. Alcohol also weakens the immune system, making it harder to fight abnormal cells.”
To explore more scientific insights, visit this detailed article on Can Drinking Alcohol Increase the Risk of Colorectal Cancer?.
Alcohol Consumption and Early Colorectal Cancer Risk
- Increased risk at younger ages: Research has shown that alcohol consumption can lead to an increased risk of colorectal cancer at an earlier age. This is a growing concern, as younger individuals continue to engage in regular alcohol use. Early-onset colorectal cancer is becoming more prevalent in those who consume alcohol frequently.
- Alcohol as a risk factor in young adults: For younger people, the long-term effects of alcohol use may lead to the development of colorectal cancer later in life. Alcohol’s effects on the digestive system over time increase the risk of early-stage cancer. Reducing alcohol consumption can help mitigate this risk.
Alcohol Consumption and Early Colorectal Cancer Risk by Ethnicity
- Ethnicity and alcohol-related colorectal cancer: The connection between colorectal cancer and alcohol use varies among different ethnic groups. For some populations, alcohol consumption has a stronger correlation with colorectal cancer, while others are less affected. Understanding these differences is key to addressing health disparities.
- Genetic differences in alcohol metabolism:Different ethnic groups metabolize alcohol in varying ways, which can influence the development of colorectal cancer. This connection between colon cancer and alcohol abuse underscores the importance of understanding genetic predispositions in the context of cancer risk
- Cultural differences in drinking habits: Social and cultural factors influence alcohol consumption patterns, which may explain some of the differences in colorectal cancer rates among different ethnic groups. Understanding these factors can help tailor more effective prevention strategies for colorectal cancer and alcohol consumption populations to molecules.
Can Genetics Affect Alcohol-Related Colorectal Cancer?
- Genetic factors in cancer risk: Genetics play an essential role in how alcohol-related colorectal cancer develops. Certain genetic mutations can make individuals more susceptible to the harmful effects of alcohol. People with a family history of cancer or specific genetic variations may have an increased risk of developing colorectal cancer from alcohol use.
- Inherited mutations and alcohol: Certain inherited mutations, such as those affecting alcohol dehydrogenase (the enzyme that helps metabolize alcohol), can make people more vulnerable to the cancer-promoting effects of alcohol. These mutations, combined with alcohol consumption, may significantly increase the likelihood of colorectal cancer and alcohol use.
- Personalized prevention strategies: For individuals with genetic predispositions, reducing or eliminating alcohol use can be an effective way to lower the risk of developing colorectal cancer. The combination of genetic testing and lifestyle changes can help decrease the chances of developing this type of cancer.
Does Stopping Drinking Alcohol Affect Colorectal Cancer Risk?
- Positive effects of quitting alcohol: One of the best ways to lower your risk of colorectal cancer is by stopping alcohol consumption. Once alcohol intake is reduced or eliminated, the body begins to heal, and the risk of developing colorectal cancer decreases significantly.
- Decreased inflammation and cell damage: Stopping alcohol consumption reduces inflammation in the digestive system, helping to repair the damage caused by alcohol. This reduces the likelihood of cancer cells forming in the colon or rectum. The longer an individual refrains from drinking, the greater the reduction in colorectal cancer and alcohol use risk.
- Improvement in overall health: Quitting alcohol benefits more than just colorectal cancer risk. It improves overall health, boosts immune function, and lowers the risk of various cancers, including colorectal cancer.
How to Prevent Colorectal Cancer
- Limit alcohol consumption: Reducing alcohol intake is crucial to lower the risk of colorectal cancer.
- Eat a healthy diet: A diet rich in vegetables, fruits, and whole grains promotes gut health. Take our Digestive and Gut Health Test in Chennai to assess your current gut condition and personalize your preventive strategy.
- Exercise regularly: Physical activity is essential for maintaining overall health and preventing colorectal cancer.
- Get screened: Regular screenings are an important step in early detection.
Conclusion
colorectal cancer and alcohol use are closely linked. Reducing alcohol consumption and leading a healthy lifestyle are crucial steps in lowering your risk of developing colorectal cancer. If you have concerns about alcohol use and colorectal cancer, we encourage you to reach out to The Arc Gut Clinic for more information and personalized guidance. We are here to support your health journey. For more information on alcohol use and colorectal cancer please contact The Arc Gut Clinic. We are dedicated to providing the resources and support you need to make informed decisions about your health.
Read also Risk of colon cancer by age