Endoscopic therapy for peptic ulcer bleeding is one of the most important tools doctors use today to stop dangerous stomach bleeds. Imagine feeling sudden stomach pain and finding blood in your stool or vomit. It sounds scary—and it is—but the good news is that doctors now have a way to fix this without surgery. In this blog, you’ll learn what happens during this type of treatment, when it’s used, and what to expect if you or someone you love ever needs it.
When is an endoscopy needed for an ulcer?
Doctors usually suggest an endoscopy for peptic ulcer disease when the patient has symptoms like:
- Blood in stool (black or tarry stools)
- Vomiting blood (looks like coffee grounds)
- Severe stomach pain that doesn’t go away
- Feeling dizzy or weak due to blood loss
These are signs of bleeding, and that’s when endoscopic therapy for peptic ulcer bleeding might be the next step. The doctor inserts a thin, flexible tube with a camera (called an endoscope) through the mouth to look inside the stomach. This helps spot where the ulcer is bleeding. Catching it early is important because bleeding ulcers can be life-threatening.
Key Takeaways:
- Endoscopy is needed when ulcers cause bleeding.
- Symptoms include vomiting blood or black stools.
- Early diagnosis can save lives.
What happens with an endoscopy?
Before the procedure, the doctor will give you medicine to relax. You stay awake but feel sleepy. Then the doctor slides a thin tube with a light and camera into your mouth, down your food pipe, and into your stomach.
This tool helps the doctor see if there’s an ulcer and where it’s bleeding. The camera sends live images to a screen so the doctor can watch closely. It may feel weird, but it doesn’t hurt. The whole process usually takes 15 to 30 minutes. After it’s done, you’ll need someone to take you home.
Many people ask, “does endoscopy treat ulcers?” The answer is yes, especially when the ulcer is bleeding. It’s a key step in ulcer treatment endoscopy. While it can also diagnose ulcers, the real magic is that it can stop bleeding on the spot.
Key Takeaways:
- A small camera helps doctors see ulcers inside your stomach.
- The test is quick and safe.
- Yes, endoscopy can treat ulcers too.
Endoscopy to treat a bleeding ulcer
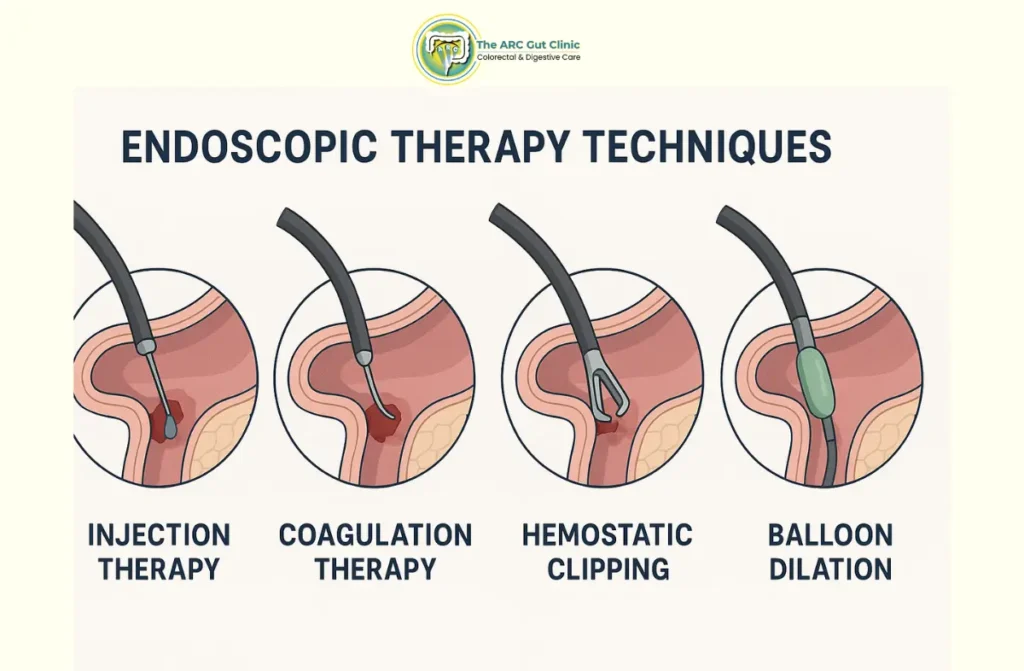
Endoscopic therapy for peptic ulcer bleeding works by stopping the ulcer from bleeding. During the endoscopy, the doctor may do one or more of the following:
- Inject medicine directly into the ulcer
- Use heat or electricity to seal the bleeding vessel
- Clip the blood vessel shut using tiny metal clips
These methods are called therapeutic endoscopy examples. They’re safe and quick. The goal is to avoid surgery and stop the bleeding before it causes serious harm.
Endoscopy for peptic ulcer disease isn’t just for checking ulcers anymore—it’s for treating them too. If caught early, bleeding ulcers can be managed entirely through this method.
Key Takeaways:
- Doctors can stop bleeding during an endoscopy.
- Techniques include injection, heat, or clips.
- Avoids the need for surgery in most cases.
How else are stomach ulcers treated?
Besides ulcer treatment endoscopy, doctors often use medicine to treat ulcers. These include:
- Proton pump inhibitors (PPIs) to reduce acid
- Antibiotics if an infection called H. pylori is present
- Medications to protect the stomach lining
Lifestyle changes are also important:
- Quit smoking
- Avoid NSAIDs (painkillers that irritate the stomach)
- Reduce alcohol
- Eat small, balanced meals
Still wondering, “does endoscopy treat ulcers?” Yes, it treats bleeding ones. But medicine helps the ulcer heal long-term and prevents future issues. You may need to keep taking medicine for weeks or months.
Key Takeaways:
- Medications are used to heal ulcers and prevent them from returning.
- Avoid things that irritate the stomach.
- Endoscopy is mainly for bleeding ulcers.
When is it necessary?
Endoscopic therapy for peptic ulcer bleeding is necessary when the bleeding is active or recent. Doctors use it:
- When bleeding is ongoing and causing low blood pressure
- If there’s a large ulcer at risk of bleeding again
- When a person shows signs of shock or fainting
Waiting too long can be dangerous. The body loses too much blood, which can lead to emergency surgery or even death. That’s why quick action through endoscopy for peptic ulcer disease is key. It’s faster, safer, and often avoids bigger problems.
Key Takeaways:
- Urgent cases need immediate endoscopic therapy.
- It’s best when bleeding is ongoing or risky.
- It can prevent serious complications.
Procedure
The ulcer treatment endoscopy process is simple but powerful. It goes like this:
- The patient is given sedative medication.
- A small tube with a camera is passed into the stomach.
- The bleeding ulcer is located.
- Tools inside the tube are used to stop the bleeding.
Therapeutic endoscopy examples used during the procedure include:
- Heat probe (cauterization)
- Injection of adrenaline
- Application of metal clips
This is done in a hospital by trained specialists. The patient may stay overnight, depending on how much bleeding occurred.
Key Takeaways:
- It’s a fast and safe procedure.
- Sedation keeps you comfortable.
- Several techniques stop the bleeding.
Risks and Complications
Endoscopic therapy for peptic ulcer bleeding is generally safe and effective, but like all medical procedures, it carries certain risks and potential complications. These depend on the patient’s condition, the extent of the ulcer, and the type of endoscopic intervention used.
- Bleeding Recurrence: Even after successful endoscopic therapy for peptic ulcer bleeding, rebleeding can occur within 48–72 hours, particularly in patients with large or deep ulcers. Careful post-procedure monitoring is essential to detect and manage early signs of recurrent bleeding.
- Perforation Risk: During endoscopy for peptic ulcer disease, there is a slight risk of perforation (a small hole in the stomach or duodenal wall), especially when thermal or mechanical methods are applied to stop bleeding. Prompt surgical or endoscopic repair is often necessary to prevent infection.
- Infection and Inflammation: Though rare, infections may develop at the site of ulcer treatment endoscopy. Preventive antibiotics and sterile techniques during the procedure help minimize this risk.
- Cardiorespiratory Complications: Sedation used during endoscopy may cause breathing or heart rhythm issues in elderly or medically compromised patients. Continuous monitoring during and after the procedure ensures early detection and intervention.
Treatment
Endoscopic therapy for peptic ulcer bleeding aims to achieve hemostasis, promote healing, and prevent recurrence. Depending on the ulcer’s size, location, and cause, multiple therapeutic endoscopy examples may be employed.
- Injection Therapy: Epinephrine or sclerosant agents are injected into or around the ulcer to constrict blood vessels and reduce bleeding. This method is often combined with other techniques to enhance long-term results.
- Thermal Coagulation: Using heater probes or bipolar electrocoagulation, the bleeding site is cauterized, effectively sealing the vessel. This is a standard approach during ulcer treatment endoscopy to achieve immediate hemostasis.
- Mechanical Hemostasis: The use of endoscopic clips or bands physically compresses the bleeding vessel, ensuring durable control. This method has proven particularly effective in large peptic ulcers with visible vessels.
- Combination Therapy: Modern approaches often combine injection and mechanical or thermal methods for superior outcomes. Studies show that combination therapy reduces the need for repeat procedures and improves ulcer healing rates.
Postendoscopic Period
The postendoscopic phase is crucial for ensuring recovery, minimizing complications, and preventing recurrence. Patients are closely monitored, and specific care protocols are followed to ensure successful outcomes.
- Observation and Monitoring: After endoscopic ulcer surgery, patients are usually observed for 24–48 hours to ensure stable vital signs and the absence of rebleeding. Medical teams evaluate hemoglobin levels, stool color, and pain symptoms to identify early complications.
- Medication Management: Proton pump inhibitors (PPIs) are prescribed to suppress acid production and facilitate mucosal healing. In patients with Helicobacter pylori infection, antibiotics are added to prevent recurrence after ulcer treatment endoscopy.
- Dietary Adjustments: A soft or liquid diet is recommended for the first few days to reduce gastric irritation. Gradual reintroduction of solid foods is guided by tolerance and recovery progress.
- Activity and Recovery: The Endoscopic ulcer surgery recovery time typically ranges from a few days to two weeks, depending on the ulcer’s severity and the patient’s general health. During this period, physical strain and stress should be minimized to support healing.
- Follow-Up Evaluation: Follow-up endoscopy for peptic ulcer disease is often advised after 6–8 weeks to confirm complete healing and to rule out underlying malignancy in gastric ulcers. Early follow-up enhances long-term prognosis and prevents recurrent bleeding.
The Endoscopic ulcer surgery recovery time emphasizes not only physical healing but also lifestyle modifications, including avoiding NSAIDs, alcohol, and smoking, to sustain ulcer remission and improve digestive health.
Conclusion
Endoscopic therapy for peptic ulcer bleeding is a modern solution that helps people recover without surgery. It’s fast, safe, and works well when used early. Whether you’re bleeding, in pain, or at risk—this method could save your life. Don’t ignore stomach pain or bleeding. Talk to a doctor and act fast.
If you or someone you love is facing a stomach ulcer, endoscopic therapy for peptic ulcer bleeding could be the best step forward. Stay informed, stay safe.
Read also Ileostomy Surgery in Chennai.




